225 years ago, the English country doctor Edward Jenner provided the first evidence that vaccination was effective. Since then, millions of lives have been saved in this way. Jenner’s approach: a person becomes infected with a harmless disease and thereby acquires immunity to a related pathogen. Back then it was probably an infection with cowpox that protected against smallpox. The term vaccine is derived from the Latin “vacca” (cow).
On July 1, 1796, the country doctor from Berkeley, England, infected eight-year-old James Phipps with smallpox virus after giving him cowpox virus a few weeks earlier. The attempt was risky – but it was successful. Phipps turned out to be immune to the dreaded disease.
Vaccines still work in a similar way today, as Adrian Hill, director of the Jenner Institute at Oxford University, explains. But they are specifically designed for this and are optimized to have few side effects and to protect them as best as possible. Hill and his colleagues developed the AstraZeneca coronavirus vaccine, which uses a cold virus in chimpanzees to carry genetic material from the coronavirus. “We use a person’s immune system to protect them,” said Hill. The knowledge that knowingly induced infection can lead to immunity to disease is very old. The so-called variolation was probably already carried out in medieval China. But that didn’t always go well.
The first vaccination clinic opens
Long unknown in the West, the method of variation came to England in the 18th century. Jenner realized it could be improved and found a source for his experiment in a milkmaid who had contracted the harmless cowpox from her cows. In a hut he called the “Temple of Vaccinia”, he opened the first vaccination clinic and made the method known worldwide. But it would take around 180 years before smallpox was actually eradicated. In 1980 the WHO declared smallpox extinct. Despite this success, there are still many infectious diseases that kill millions each year. The worst killers include tuberculosis, malaria and HIV / AIDS, for which widely available and effective vaccines are still not available.
Hill and his colleagues have developed a malaria vaccine that meets WHO standards with over 75 percent effectiveness. But it will take years before it can be used across the board. A lengthy approval process is required.
Hill finds this inappropriate given the speed at which coronavirus vaccines have been approved over the past year. In Africa, four times as many people died of malaria last year than Covid-19, he says. Even so, do not treat the disease with the same urgency.
It’s all a matter of money
In addition to the tough approval processes, a lack of funds for the development of vaccines and a lack of production capacities are primarily responsible for the fact that things do not move faster. “If you knew you could sell a tuberculosis vaccine for $ 100 a dose, all the big drug companies would be doing it today,” says Hill. Research is in competition with other, less fatal ailments. But the deadliest infectious diseases occur mainly in less financially strong developing countries.
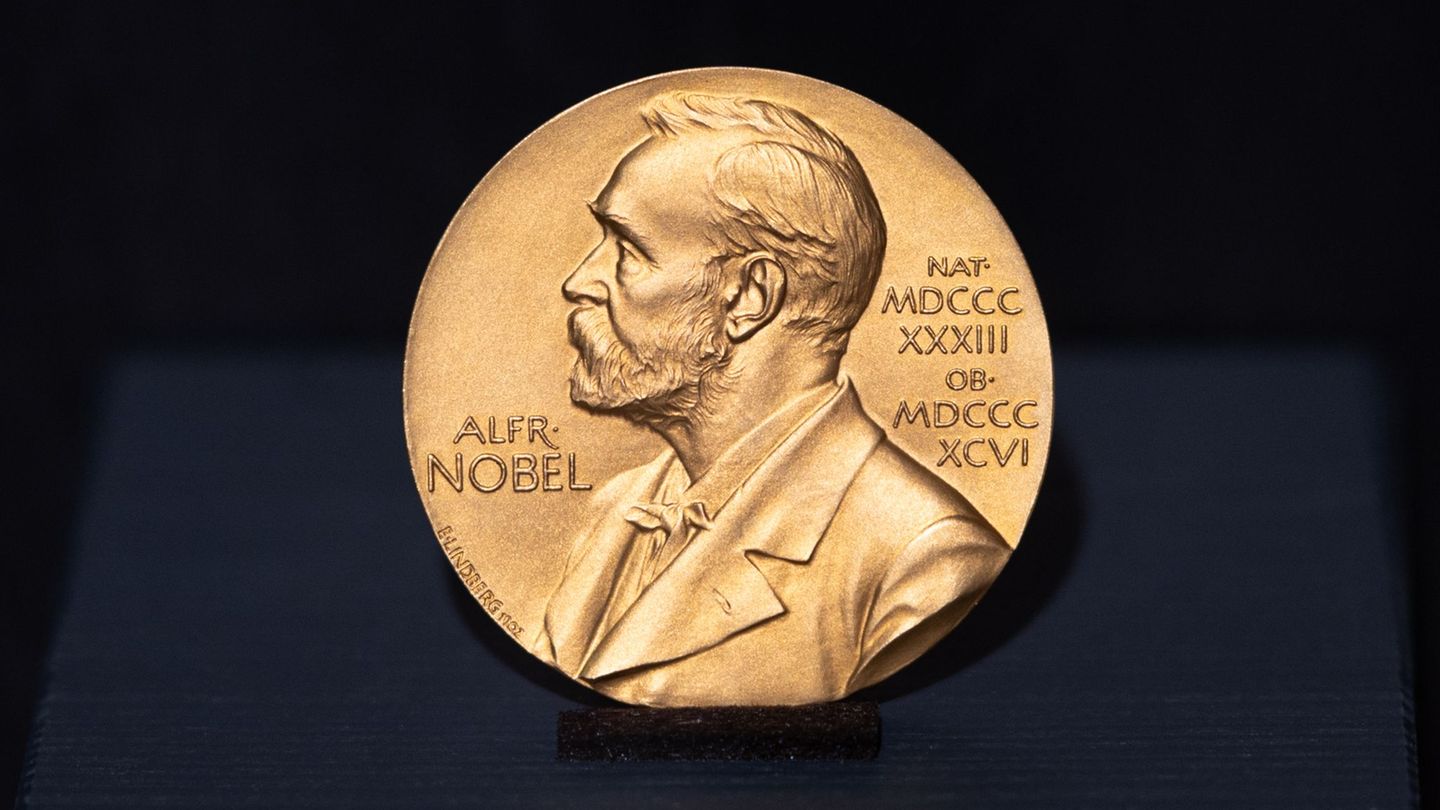
Vaccination pioneer Edward Jenner was never interested in making money from his discovery. Jenner had an absolute will to save as many lives as possible, said Owen Gower, museum director Dr. Jenner’s House in the Berkeley country doctor’s former home.
I am Pierce Boyd, a driven and ambitious professional working in the news industry. I have been writing for 24 Hours Worlds for over five years, specializing in sports section coverage. During my tenure at the publication, I have built an impressive portfolio of articles that has earned me a reputation as an experienced journalist and content creator.