The latest Omikron variant BQ.1.1 could soon cause a next wave and thus bring more patients into the clinics and cause staff shortages. The clinics are facing a hard winter – according to physician Christian Karagiannidis. What the hospitals urgently need.
It is currently still being discussed whether the facility-related vaccination requirement for health workers will be extended or not. But according to experts, it is not an instrument to relieve the clinics this winter. With rising energy costs and the threat of flu and corona waves, German clinics are faced with other problems.
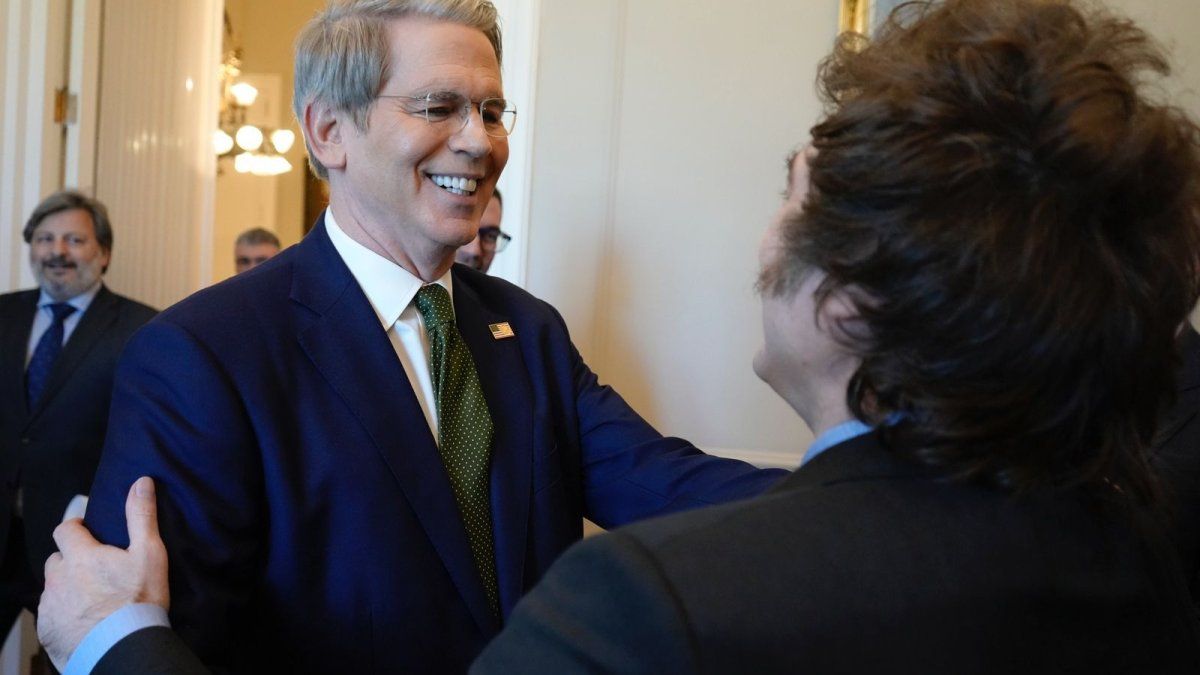
In contrast to the last pandemic years, the situation this winter has become much more complex, says Professor Christian Karagiannidis in an interview with the star. He is a pneumologist and intensive care physician at the lung clinic of the Cologne Clinics and a member of the Corona Expert Council of the Federal Government.
“In the last pandemic winters, we only had Covid-19, so to speak. This winter, Sars-CoV-2 will bring fewer patients to the intensive care unit, but lead to significantly more staff absences. At the same time, we will probably see influenza and other respiratory infections. The result : More patients are coming to us and at the same time more staff will be absent.” In addition, hospitals could get into financial difficulties due to inflation and the energy crisis. In addition to the rising costs, clinics would face a loss of income – also caused, among other things, by the acute and chronic shortage of staff.
Federal Minister of Health Karl Lauterbach wants to get the problems caused by the rising costs under control with the Economic Stabilization Fund. Money is to be made available to hospitals from this fund. “No hospital will have a problem because it cannot pay for inflation, electricity or gas,” said the SPD politician.
Corona situation currently acceptable in the hospitals
The corona situation in the clinics is currently acceptable, but there are already significant regional burdens, especially in the normal wards, says the expert. According to the German Hospital Society, the number of corona-positive patients in the normal wards has fallen by around 15 percent and in the intensive care wards by ten percent compared to the previous week. Due to the holiday, the data might be slightly skewed.
But recently the trend could be observed that patients who had to be treated in hospital for another illness tested positive for Corona during their stay. For doctors and nursing staff, this means a considerable amount of extra work: “We have to isolate all Covid 19 patients. Every time you go into the patient’s room, you always have to dress completely in protective clothing. So one Put on a plastic apron, gloves, face mask and hood. Even if there is an emergency in the room, I cannot just walk into this room – I have to get fully dressed first. That makes a big difference when there are many patients are”, describes Christian Karagiannidis.
Another problem: “During the pandemic, we saw that the underlying disease, which is why a patient comes to the hospital, deteriorates significantly due to the corona infection. It is therefore important that we also know the secondary diagnosis with Covid-19 very much take seriously.” If corona patients have to be treated in the intensive care unit, they still have a very bad prognosis, says Christian Karagiannidis. “The patients are in the intensive care unit for a very long time and they are also going through what we have been through in the last pandemic years with Omikron.” It is positive that there are far fewer cases that develop pneumonia than with previous corona variants.
If we expect a pronounced flu epidemic this winter, as many experts suspect, the staff in the clinics will have even more work to do. Because: “Even in the case of flu, the patients must be isolated and quite a few can become seriously ill.”
Risk groups should be vaccinated against influenza and pneumococci
Christian Karagiannidis therefore emphasizes the importance of vaccination against influenza and pneumococci – especially for risk groups. “It’s very important for the clinics so that we don’t get so many serious cases.” Christian Karagiannidis, on the other hand, does not consider the continuation of compulsory corona vaccination in hospitals to be elementary in order to relieve the burden on the clinics. “We have extremely high vaccination rates nationwide in the inpatient sector – compulsory vaccination does not play a major role here.” The expert also does not consider daily tests for the staff to be necessary this winter. “With the rapid tests, we can only filter out staff who have a high viral load anyway, and I refuse a daily PCR test.” It is much more important that doctors and nurses wear their masks correctly, so the probability of infection is very low – even if someone is infectious.
In the face of a harsh winter, hospitals across the country would have to prepare in such a way that they can provide good care to all emergency patients. Clinics should therefore network well so that patients are well distributed in a region. It will also happen this winter that normal day-to-day business with many routine interventions cannot be maintained as doctors would like. It is a big problem that the workforce has become extremely thin, describes Christian Karagiannidis. “We noticed in the summer wave and also in the fall that we couldn’t operate beds because all of the staff’s compensation mechanisms had been used up.”
Clinics urgently need reforms
The pandemic has once again highlighted the weaknesses of the health system. “Since the introduction of the flat rate per case 20 years ago, there have been no real pioneering reforms in the healthcare system.” This means that hospitals can only bill the health insurance company for cases that are remunerated at different rates. Talking medicine or even good care is hardly or not at all remunerated. “No reforms have been made even though we know this system is going in the wrong direction and even though we’ve known for 20 years that there is a demographic tsunami ahead. What I mean by that is that demographics are definitely causing us to lose more nurses “At the same time, we will have more older patients and fewer contributors. We should have initiated reforms ten years ago. We can only get out of this whole mess if the healthcare system is fundamentally reformed,” says the expert. Christian Karagiannidis does not want to demonize a certain economy – but in Germany we have the absolute extreme form of it.
Health Minister Karl Lauterbach wants to reform the health system. The outpatient and inpatient care should be better interlinked. In addition, obstetrics stations are to be secured and children’s hospitals are to be relieved. The Minister of Health announced that the flat rate per case at the children’s hospitals would be overcome. However, hospital planning is in the hands of the federal states – so the federal government cannot decide alone at this point.
The sick person is overlooked too much in the healthcare system
“A basic problem of the current system is that many health economists and decision-makers think far too technocratically and not enough humanistically. The humanistic approach has been lost in the last 20 years. There is far too little orientation on the fact that there is a sick human,” says Christian Karagiannidis. So that means: It is oriented far too much to large, well-paid services and necessary discussions would not fit into this system. It is also important that, similar to the fire brigade, the provision is also paid for. So it would also have to be paid that hospitals with a high degree of specialization are maintained and people work there permanently and not only the treatment is remunerated.
In view of the aging population, the expert believes that small clinics in particular need to be converted into outpatient and inpatient centres. “I imagine a modern concept with acute care and the integration of resident doctors. A place where the primary concern is that the elderly and/or people in need of care receive human and nursing care.” He doesn’t think much of the idea of closing all small hospitals. The fact that there are so many hospitals in Germany is a huge opportunity to be able to provide good care for older patients outside of the metropolitan areas, they just have to change. Because: “Dementia patients in particular have a care requirement that is comparable to that of a small child. We would need a lot more staff to take care of the patients. The basic idea in the broad care of the older population is that the staff has time for the people and is not busy carrying out thousands of tests on them,” says Christian Karagiannidis.
Source: Stern