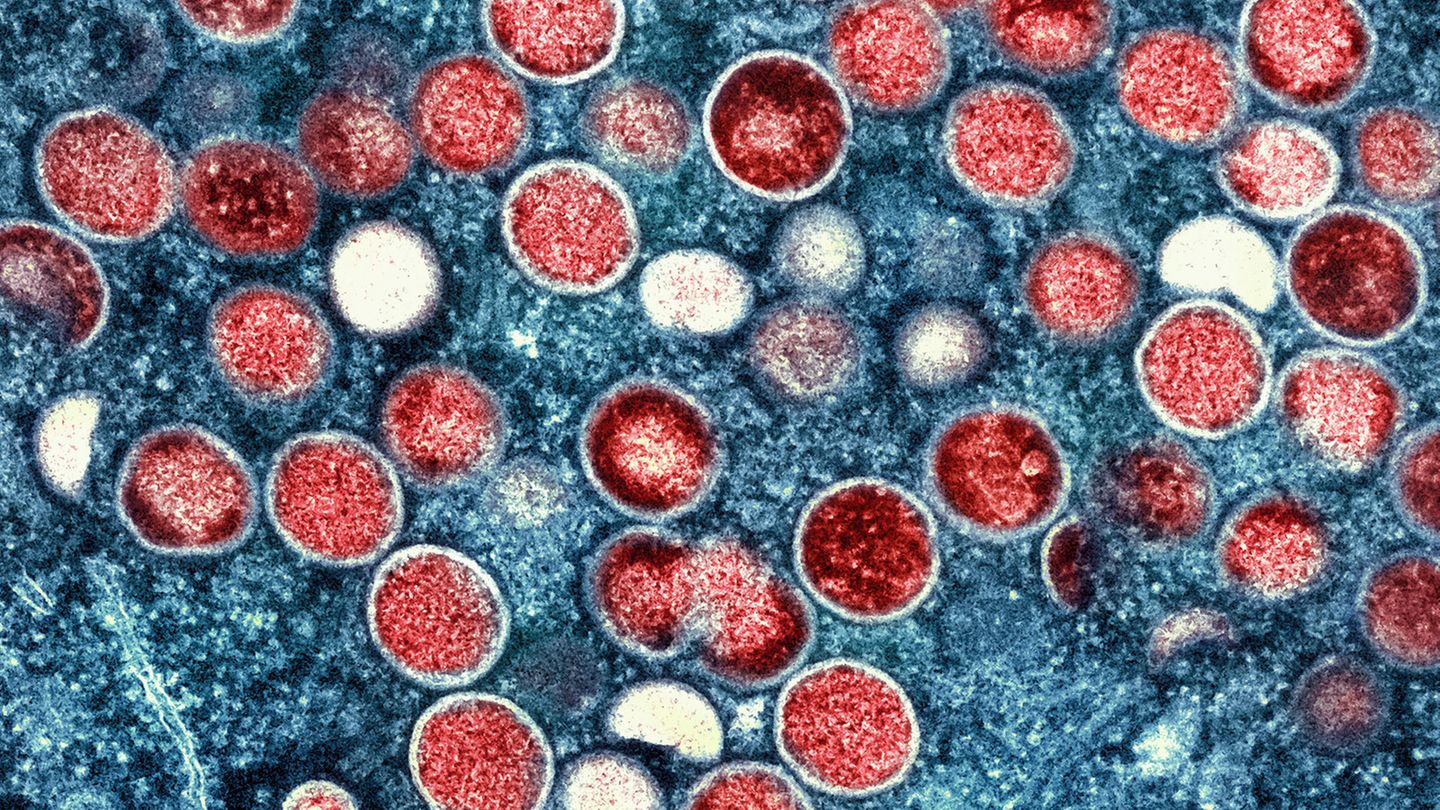
The World Health Organization recently declared an international public health emergency because of Mpox. Why we should keep a close eye on the virus.
The numbers alone show how worrying the situation on site is. The African Union Health Agency (Africa CDC) has recorded over 42,000 cases of Mpox – formerly “monkeypox” – since the beginning of the year, significantly more than in the whole of last year. But an increase of almost 80 percent compared to 2022 had already been observed. Since then, the number of infections has increased exponentially. Almost all cases, including the 1,100 fatal ones, currently come from Central Africa. The first infections are also occurring in other parts of Africa. One day before the WHO’s decision, the Africa CDC had declared a state of emergency for the entire continent for the first time.
How Mpox (“monkeypox”) is transmitted
Infection occurs through close contact with infected animals or people. After an incubation period of 5 to 21 days, symptoms of the disease may appear, usually pox-like rashes, either locally or all over the body. The vast majority of sick people get over it after two to four weeks. However, there are also severe cases with high fever and swelling of the lymph nodes and, in the worst case, fatal infection of the organs, especially the spleen and liver.
The African experts see frequently changing sexual contacts, co-infections with HIV, for example, as well as malnutrition and the associated immune deficiency as crucial risk factors. Sex workers and their customers or men who have sex with men often become ill. The latter group in particular was affected in Western countries during the 2022 outbreak.
Because MPXV, the abbreviation for the virus, was first discovered in monkeys from Singapore in 1958 in a Danish laboratory, but monkeys are not the main carriers of this virus in nature, the WHO has given the long-used name “monkeypox” at the end of 2022 replaced by the neutral “Mpox”, which is now also common for us. The virus probably passed to humans decades ago via domestic rodents. The first cases were discovered in several African countries in the 1970s. Children were also often affected, probably because they picked up the pathogen through the excrement of infected rodents while playing. Sex is therefore not a prerequisite for infection, although it is probably the most common route of transmission. And each new transmission gives the pathogen the chance to change and adapt to new conditions.
Based on its genetic makeup, the virus can be divided into two groups, which are technically called “clades”. These virus families, referred to with Roman numerals as clade I and clade II, are so similar to each other that the MPXV genome sequences, consisting of around 200,000 genetic “letters”, are more than 99 percent identical to one another. And the similarity to other types of smallpox is over 90 percent.
But even the small difference can have significant consequences. This is particularly true with regard to the course of the disease. Clade II viruses are usually more harmless. It was such viruses (“clade IIb”) that led to the major outbreak in West Africa in 2022 and 2023 and ultimately to almost 100,000 infections in a total of 116 countries worldwide. Germany was also affected with around 3,800 cases, most of them between June and September 2022. After that, Mpox was only diagnosed sporadically in our country. In Africa, however, new cases continued to occur in larger numbers.
More dangerous viruses are currently circulating
This time it is the more dangerous viruses of clade I that are becoming increasingly widespread in Africa. In the Congo Basin, a mortality rate of just over 3 percent of cases was observed for this genetic group. In the past, however, there have been case fatality rates of almost 11 percent. In clade II, on the other hand, only around 0.2 to a maximum of 3.6 percent of the infections were fatal. But viruses change. As early as April, samples from the Kamituga mining region in the east of the Democratic Republic of Congo revealed Mpox pathogens from a new subvariant from clade I. This new genetic group is now called “clade Ib.” Not only are the disease processes caused by it generally more serious than in clade II. Within clade I, mutations are now evident in a region of the genome that particularly promotes infection from person to person. The virus continues to adapt to its new host.
As early as 2022, a Portuguese research team had discovered a mutation rate in this genetic region of the Mpox virus that was six to twelve times higher than would be expected from experience with such smallpox viruses. Mutations occur randomly, like typographical errors, and the virus often cannot survive such genetic mistakes. However, this can also result in a mutant that has an evolutionary advantage and can, for example, be transmitted more easily from person to person than older viruses of this type. Unfortunately, this seems to be the case with the Ib clade now spreading across central Africa. Based on the known mutation speed and in comparison with previous samples, it can be assumed that this subvariant of MPXV first appeared in July 2023 at the earliest and has been spreading since then.
WHO has declared a global health emergency
So it is only logical that authorities such as the Africa CDC and the World Health Organization (WHO) are closely monitoring developments and are now taking precautions to contain them as quickly as possible. Above all, the WHO now wants to prevent the virus variant from clade Ib from spreading globally and has declared a global health emergency. This is the highest warning level available to it according to its statutes, official name: “Public Health Emergency of International Concern” (PHEIC), i.e. a health emergency of international concern. Covid-19 also had this official status.
But in the case of Mpox, this is by no means the same as a new pandemic, but above all gives the WHO the opportunity to act in an internationally coordinated manner to prevent anything worse from happening. The WHO Director-General and all 194 contracting states are legally obliged to implement the recommended measures of an emergency committee made up of appropriate experts. Both the US infection control agency and its European counterpart currently consider the danger from the new Mpox sub-variant to be very low in their respective regions. But it would be fundamentally wrong to sit back and relax. Because the virus doesn’t take a break either.
That is why the WHO recently presented a strategic framework for the global containment and control of Mpox for the coming years up to 2027. There is already an effective vaccine, even if exact figures for such a supposed niche product are missing. A more recent review article, in which the studies available to date were evaluated, comes to almost 60 percent protection against severe symptoms. No serious side effects were observed. However, it is not clear to what extent the vaccine itself reduces the risk of infection. “Imvanex” is the only smallpox vaccine approved in the EU, but was not available during the 2022 outbreak, for example. So a closely related product from the same manufacturer (Bavarian Nordic A/S) had to be used and imported from the USA under the name Jynneos. But these stocks were also very limited due to the sudden global demand. On September 5th, the first 200,000 doses from the EU arrived in the Democratic Republic of Congo, plus 65,000 doses from the USA. Nigeria had already received 10,000 doses of Jynneos in August.
Bottlenecks in the supply of vaccine must not be repeated. There is also a lack of additional studies on the likely diminishing effect of the vaccines. Better vaccines should be developed and, if possible, antiviral drugs, says the WHO in its precautionary plan. After all, a PCR test has already been presented that can fish out the new viruses of clade Ib from their genetic relatives and track their further spread.
Yes, all of this costs. But Mpox are a good example of why pandemic preparedness is an essential investment in the future – and why it can be very dangerous to put off such investments. If it isn’t the Mpox pathogens that surprise us tomorrow, then perhaps it will be bird flu or some virus that no one knows about yet. The US virologist Anthony Fauci, known worldwide for his HIV research and the corona pandemic, once summarized it as follows two years ago in a warning article for the “New England Journal of Medicine”: “It’s not over until it’s over …but it’s never over.”
Note d. Editor: This article first appeared on stern Plus on August 10, 2024 and has been updated.
Source: Stern
I’m Caroline, a journalist and author for 24 Hours Worlds. I specialize in health-related news and stories, bringing real-world impact to readers across the globe. With my experience in journalism and writing in both print and online formats, I strive to provide reliable information that resonates with audiences from all walks of life.