Some injuries, such as spinal cord injuries, can compromise mobility permanently, but not in all cases. Complementary neurophysiological studies should not be delayed since they will not only provide the patient with a prognosis, but will also give surgeons a clue about the approach to follow in each case.
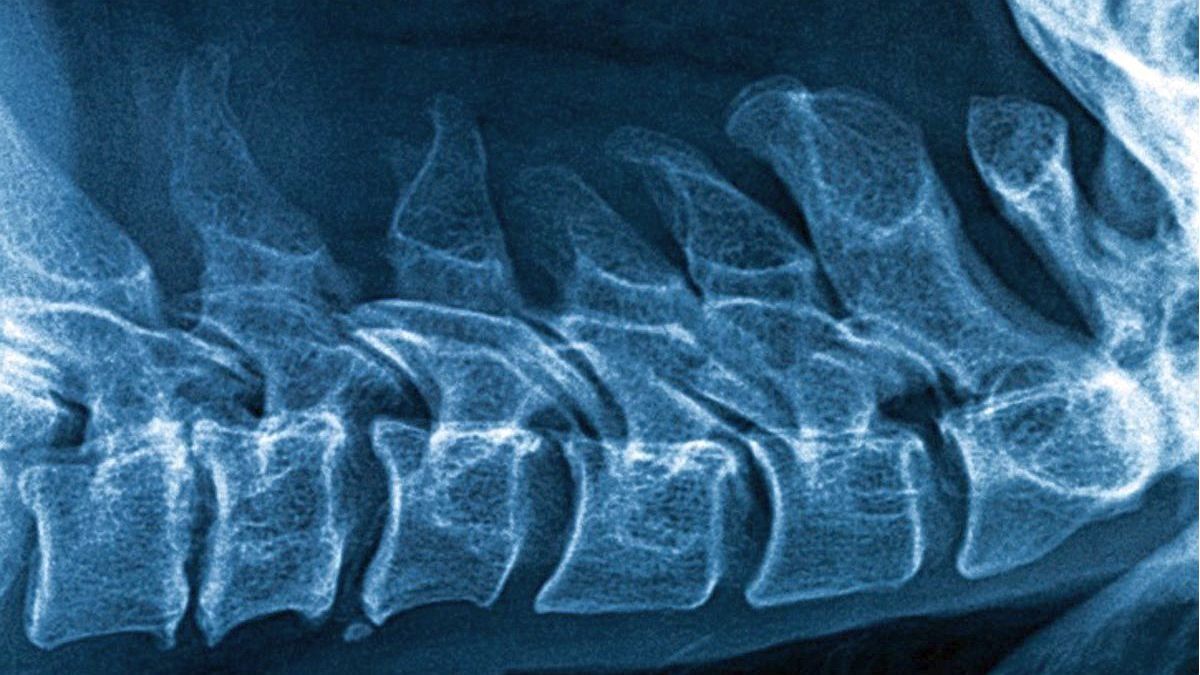
Injuries, whether from sports or traffic accidents, are the main cause of spinal cord injuries in young patients, while in adults they can also occur due to osteoarthritis (when the spinal cord narrows in the cervical spine, for example), herniated discs or tumors.
When they occur due to blows, it is important to carry out neurophysiological studies as soon as the patient arrives at the hospital, because with that information the course of action to be followed will be marked. Specifically, they cannot miss the somatosensory evoked potentials (SSEP)which evaluate the nerve transmission of impulses in the somatosensory pathways of the extremities (upper and lower) and in the brain, and can be used to diagnose injuries at the level of the nerve roots, the spinal cord and the brain.
It is important that these studies are requested and not be left alone with the resonance. To explain how both exams complement each other, I usually choose the metaphor of the wall of a house. MRI would be the equivalent of photographing a damp patch, while somatosensory evoked potentials would be the equivalent of visiting the electrician to check the “wiring” that passes through it.
With SSEP, the function of the spinal cord itself is evaluated: it confirms whether the transmission of impulses occurs even after an injury or a narrowing of the canal. These tests can be supplemented by electromyography, which analyzes the electrical activity of muscles and nerves and with the study of spinal cord reflexes.
In the specific case of traumawhy is it important to order the SSEP as soon as the patient enters the hospital? Because at the moment of the modular lesion, the first thing that happens is the so-called spinal cord shock (flaccid paralysis or loss of spinal reflexes), which are comparable to when a boxer does not react after a blow and is as in knock out. The same thing happens in the spinal cord: at the moment of impact it does not react, but that does not mean that it has been sectioned and lost its function, but rather that in some cases it can be recovered little by little.
Let us give two examples of patients who arrive at the emergency room after motorcycle accidents. They cannot feel their legs and cannot move them due to spinal cord shock. Somatosensory evoked potentials are performed on the first and it is verified that the medulla retains some degree of function. So in that case the first thing to do is decompress the spinal cord, which is inflamed within the medullary canal. So that this marrow does not lack oxygen (what is called marrow anoxia) and can expand in a certain area, a laminectomy, that is, to remove the “roof” from the medullary canal. In this case spinal cord function is prioritized over spinal stability, and stabilization surgery is performed in a second stage.
Another patient, also fractured, arrives without feeling his limbs either, but the somatosensory evoked potentials are negative, they do not record spinal cord function, so that means that the medulla is sectioned. In these cases, as there is no possibility of regaining mobility, which must be prioritize is to stabilize the spine, because an unstable spinal cord can lead to additional complications. In addition, having the results in advance will help professionals to break the news in time, both to the patient and to their relatives.
In short, the somatosensory evoked potentials will allow the surgeon to judge what his priority will be, whether to negotiate instability to give the spinal cord a chance to recover, or to perform spinal stabilization surgery immediately.
But the somatosensory evoked potentials not only serve to know how functional the spinal cord is, but also guide the level where the lesion that produces the “stop” in the transmission is located: at the cervical, dorsal or lumbar level. Locating the problem is useful in the event that spinal cord injuries are caused by degenerative diseases.
The SSEP should always be performed by clinical neurophysiologists, who will know how to perform it correctly and who will also give an accurate interpretation of the results. If the nervous system were a cable, clinical neurophysiologists are a kind of “electricians of the body”.
Director of the Argentine Foundation for Clinical Neurophysiology, specializing in Clinical Neurophysiology (MN 103136).
Source: Ambito